Gut-Brain-Microbiome Axis
Gut-Brain-Microbiome Axis
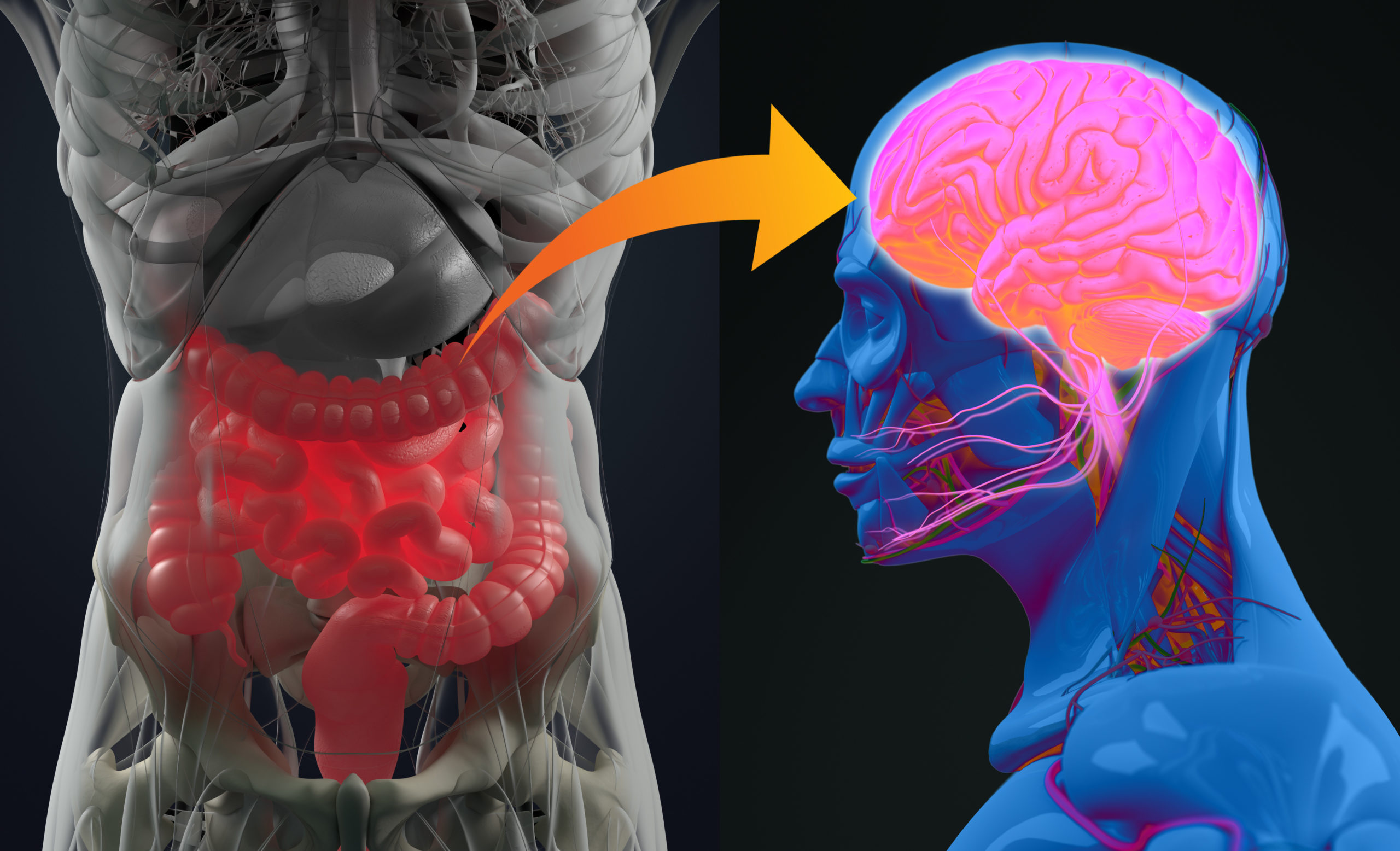
How the communication between your gut, brain, and microbiome influences IBS
Irritable bowel syndrome (IBS) has been a bit of a medical mystery between trying to find better ways to diagnose a person with IBS, pinpointing what causes IBS in the first place, and finding the best treatment options. At first, the focus was on foods by trying to determine what dietary factors made symptoms better or worse. This gave rise to restrictive diets like gluten-free diets or the even stricter low-FODMAP diet. FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols; these are just short-chain carbohydrates and sugar alcohols that are difficult for the body to break down and absorb through the small intestine. When the small intestine has difficulty absorbing nutrients it triggers a reaction that causes more water to be drawn into the lumen and expand more than normal; this sends pain signals to the brain and creates the sensation of cramps, a symptom of IBS. Studies ultimately found that the low-FODMAP diet wasn’t really any more effective than the conventional IBS diets, but it did however, lead to major changes in the microbiome of the gut.1,3 Research found that low-FODMAP diets could throw the whole gut microbiome out of balance by killing off essential prebiotics. For this reason, even though it helped some patients with their symptoms, doctors realized that it could do more harm than good as a long-term solution for treating IBS. The same study also found that humans might actually need certain FODMAPs that promote the production of good bacteria our intestines need to function efficiently.1 When scientists realized how delicate the microbiome of the gut was, they began to look at the connection between changes of microbiome health and how it affects the brain.
Good microbiota is important to the gastrointestinal tract because they work with the epithelial cells that line our intestinal wall to strengthen our immunity, digest food, absorb essential nutrients, and have now been shown in mice to directly interact with the central nervous system.2,6 The two-way connection between the digestive tract and the brain has been well established. However, the idea that microbiota may have a direct link to brain function and development, and vice versa, could lead to medical breakthroughs on how to diagnose and treat many illnesses including IBS. The evidence from studies suggests that when the balance of the microbiome within the gut is thrown off, signals are sent to your brain, via the central nervous system, to tell it that something is wrong.2,6 The vagus nerve is an important part of the central nervous system that connects the brain to the visceral organs like the heart, lungs, and digestive tract. This cranial nerve plays a big role in digestion because it sends signals from the brain to control the subconscious muscle movement of the digestive system as well as visceral sensations from the digestive system to the brain.2 It has been shown in mouse studies that because of this bidirectional connection through the CNS, microbial imbalance can directly influence a variety of brain functions such as neurological development, cognitive ability, pain sensitivity, and even mental health.2,3 Since this pathway is bidirectional, it led scientists to believe that if microbial change in the gut can affect the brain, then changes in the brain should also affect the microbiome of the gut. They realized that if their theory was correct, this connection could lead to an explanation of what causes IBS and possible treatment options. 2
Researchers have taken this theory and linked possible causes of IBS to “perturbations of the gut microbiome”.2 These changes happen from many things, but when it comes to IBS researchers have narrowed their investigation down to excessive antibiotic use, previous gastrointestinal infections, and psychosocial trauma.2 When someone has a GI tract infection, they either let the body fight the infection naturally, or sometimes an antibiotic can be prescribed to help kill off the bad bacteria in the gut causing the infection. When an antibiotic is used, it can kill off groups of good bacteria that resemble the targeted bacteria causing an imbalance in the microbiome of the gut. Microbiologist William de Vos believes that in some cases those good bacteria don’t come back, and your microbiome gets locked into a perpetually disrupted state leading to gastrointestinal disorders like IBS.2 When certain gut microbes are wiped out it can also change the intestinal environment which can lead to long-term gut hypersensitivity, impaired digestion/excretion, and lowered stress response; which are all symptoms of IBS that are connected to the brain.2,3 Animal studies have revealed that mice who don’t have a specific microbiota showed an increase in cognitive irregularities that resemble symptoms of anxiety or depression in humans.2,3 This kind of connection between the microbiota and the brain could explain why gastrointestinal disorders, like IBS, usually go hand in hand with some sort of psychiatric issue.2
Early life trauma is a psychosocial trauma commonly expected to initiate the onset of mental illnesses like post-traumatic stress disorder or depression. There is now additional research that suggests there may be a link to gastrointestinal disorders as well.2 The theory is that since this axis is bidirectional, an early life trauma that alters the brain, structurally and functionally, could potentially affect the microbiome of the GI tract enough to induce IBS. Animal studies have shown that when a mouse experiences trauma, the region of their brain that responds to pain completely changes. This change in the brain then triggers the CNS to make changes to the microbiome of the gut. Consequently, these changes to their gut microbiome lowered production levels of dopamine, adrenaline, and serotonin.2 Serotonin is an important neurotransmitter that regulates mood, regulates digestive motor function, and conveys sensory signals from the GI tract to the vagus nerve. 2,5,6 Low levels of serotonin are commonly linked to depression, but it also leads to inflammation, visceral hypersensitivity, lowered gut motility, and lowered intestinal secretion; all of which are symptoms of IBS.6 Another study revealed that in healthy mice a specific subgroup of microbiota was found that stimulated the synthesis and secretion of serotonin from enterochromaffin cells in the epithelial wall.2,5,6 The evidence that these animal studies have provided highlight how versatile serotonin can be in future diagnoses and treatment for gastrointestinal disorders in humans.
Since research has continued to strengthen the connection of IBS to serotonin fluctuations, more doctors have started using “selective serotonin re-uptake inhibitors and tricyclic antidepressants” to effectively treat IBS symptoms.5 Another treatment option that has been proven to alleviate some patient’s IBS symptoms, is giving patients a big dose of healthy probiotics to help balance out their microbiome.2 As scientists learn more about the different groups of microbiota in the human digestive system through study of biomarkers, gene sequencing, and RNA sequencing, they can begin to determine how each of them influences digestive health and brain function.4 Once scientists have that information they can use it to easily diagnose what disorder they are dealing with by knowing what type of disorder certain microbiota in the gut are associated with. Then they can develop ways to add or take out specific microbiota in an individual’s microbiome to treat various disorders, including IBS and depression3,4 It’s exciting that there is so much research going into understanding the gut-brain-microbiome axis because if scientist can solve the mystery of how both directions work in humans, IBS could be just the beginning.
References
1. DeWeerdt, Sarah. Food for thought. Nature. 2016, Vol. 533, pp. S108-S09.
2. Eisenstein, Michael. Bacterial Broadband. Nature. 2016, Vol. 533, pp. S104-S106.
3. Ghosh, Dilip. Potential Role of Microbe-Gut-Brain Axis on Mood. Nutraceuticals World. 2018, p. 40.
4. Katsnelson, Alla. Filling in the missing pieces. Nature. 2016, Vol. 533, pp. S110-S111.
5. Morgan, Branwen. A healthy pipeline. Nature. 2016, Vol. 533, pp. S116-S117.
6. Hoffman, Benjamin U. and Lumpkin, Ellen A. A gut feeling. Science. 2018, Vol. 361, 6408, pp. 1203-1204.